March 6, 2018
A CBC awardee Eugene Chang, UChicago, contributes his expertise into a discussion about the causes and treatment of IBD and other gut imbalances
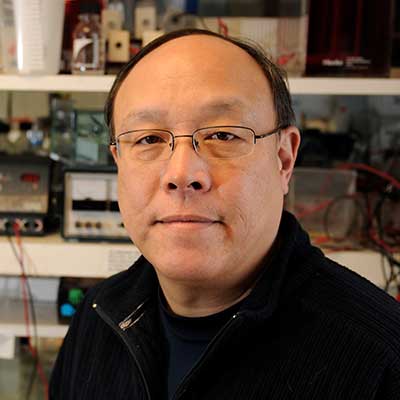
Irritable bowel syndrome (IBS), is a common chronic intestinal disorder causing abdominal discomfort and pain, gas, diarrhea, and constipation. It can be crippling to those affected with it. The pathology of IBS is not well understood and the gut tissue appears to have no underlying damage. In the article below, published in Chicago Sun Times, Eugene Chang, UChicago, an expert in the area of microbiome of a healthy and inflamed gut, discusses the current state of IBS treatment. Chang is a past CBC Catalyst Award (2015) recipient. Congratulations!
Stomach, digestive system health: What’s your gut telling you?
Chicago Sun Times | by Sandra Guy | February 21, 2018
If your digestive tract is healthy, you generally feel better. Researchers and physicians for years have been touting the importance of good gut health to a person’s overall well-being.
Those with less than optimum gut health know there’s truth to the assessment.
Case in point: A lettuce leaf can bring Danny Bernstein to his knees in excruciating stomach pain. A piece of broccoli can send him to the hospital.
Bernstein, 56, has suffered from both Crohn’s disease and irritable bowel syndrome (IBS) for 43 years, so he has had to learn which foods he can eat without doubling over in pain. He can handle bananas, for example, as long as they’re crushed in a blender or — if he has the time — can chew them well. He can eat avocados, but not onions.
Indeed, dealing with irritable bowel syndrome and other gut-related illnesses isn’t “a cookbook science,” experts say.
“It’s a lot of trial and error, and finding out what works for you,” said Kristi King, spokeswoman for the Chicago-based Academy of Nutrition and Dietetics.
Yet research shows that people who struggle with chronic diarrhea, constipation or both, can minimize their symptoms by drinking lots of water, exercising an hour a day, and keeping lists or diaries of their food intake to figure out the foods that may make them sick.
“A food diary can be important, as well as writing down the time you have symptoms, to see if there’s something you’re eating that’s making your symptoms worse,” King said.
For those with diarrhea or frequent gas — the kind that occurs at least once a week over a three-month period – the best diet is one with lots of soluble fiber (the kind that dissolves in water), such as apples, pears, carrots, berries and oatmeal.
If you have frequent constipation, the recommended diet is one with insoluble fiber, such as asparagus, celery, kale, broccoli and Brussels sprouts.
Foods to avoid include those with high fructose such as mango, cherry, pomegranate, watermelon and grapefruit, and well as high sugar-alcohol foods such as ketchup, barbecue sauce and fruit-flavored snack foods.
After visiting a doctor or a registered dietician, IBS sufferers may be guided to what’s called a low-FODMAP diet — based on fermentable, oligo-di-mono and polyol substances, King said. The six- to eight-week diet eliminates foods high in certain carbohydrates such as garlic, onions and onion powder.
In Bernstein’s case, he decided to avoid most medicines and a third surgery, and to instead concentrate on figuring out the best diet to control his pain. He eats mostly protein and a few basic starches such as white rice and corn tortillas.
His physician for Crohn’s, Dr. Steven Hanauer at Northwestern, introduced Bernstein to Dr. Laurie Keefer, now at Mt. Sinai, who helped him to understand that a primary cause of irritable bowel syndrome is neurological. IBS can cause abdominal pain, bloating, constipation and/or diarrhea as the brain overreacts to nerve signals from the gut.
“Drugs work only on the symptoms of constipation or diarrhea, not the cause of IBS,” said Bernstein. “IBS is primarily a brain-gut issue. The nerves are misfiring and the brain is sending inappropriate signals back to the gut.”
Bernstein was looking for a way to help the 20 million Americans suffering from irritable bowel syndrome.
So the former children’s video game creator licensed a clinically proven drug-free treatment and started metaMe Health, a network that connects IBS sufferers with a three-month online treatment program delivered by therapists trained in gut health. The company’s long-term goal is a digital version of the therapy. After FDA clearance of the digital treatment, he aims to reach 20,000 patients in the first year (0.1 percent of those with IBS); 200,000 (1 percent) in the second year, and 400,000 (2 percent) in year three.
Meanwhile, University of Chicago researchers are working on remedies to restore health to people’s guts, many of which are suffering mightily from America’s high-fat, high-sugar, low-fiber diets lacking in leafy greens and oversaturated with anti-microbial hand soap and antibiotic-laden meats.
The researchers agree that probiotics and prebiotics do little to help, and are unregulated, meaning that they don’t undergo the rigorous testing required of drugs that get U.S. Food and Drug Administration approval. The researchers are looking for more targeted and sophisticated solutions. Dr. Eugene B. Chang is focused on ways to ensure that people have healthy gut microbiomes — a collective of gut microbes, genes and a variety of cell types.
“A healthy gut microbiome is essential for our existence,” said Chang, a University of Chicago professor of medicine and a scientific advisory board member of the American Gastroenterological Association Center for Gut Microbiome Research and Education. “It processes food in a way that’s vital to our well-being” because of the role it plays in obesity, diabetes and inflammatory bowel diseases.
The search for a healthy microbiome has even led some companies to take healthy people’s fecal samples and them in capsule form or in a powder to mix in a cocktail, as a way to boost gut health.
Chang doesn’t disagree with the use of stool microbial capsules or even probiotics or prebiotics. But he said he believes experts “can do better — in a way that requires a more scientific and rigorous approach to establish efficacy and safety of these interventions.”
“We also have to recognize that one pill, prebiotic, probiotic or diet is not going to work for everyone and for everything,” Chang said. “We have to figure better ways to tailor these approaches to each patient.”
Chang and his research team are using technologies such as computational systems, DNA sequencing, and animal and tissue modeling to figure out the causes of IBD and other gut imbalances. They are working to develop tests to predict people’s risk for gut-related diseases and develop strategies to prevent, treat and cure them.
The best bet for people without gut diseases, for now, is to exercise, eat leafy green vegetables, foods with healthy fiber such as celery and apples, and cut the high fat and sugar, said Dr. Christina E. Ciaccio, acting chief of allergy immunology and pediatric pulmonary and sleep medicine at the University of Chicago.
“Just getting back to the basics may be what helps us in the end,” she said.
Source:
Adapted (with modifications) from Chicago Sun Times, by Sandra Guy, posted on February 21, 2018.
Ties to CBC:
CBC Catalyst Award (2015):
PIs: Hyunyoung Jeong (UIC) and Eugene Chang (UChicago) for the project:
▸ Role of Gut Microbiota in Determining Drug Efficacy and Toxicity